Depression is a condition affecting millions of people worldwide. It can be hard to recognize at first since depression often masks itself behind many different symptoms, including mood swings, irritability, and an overall sense of sadness or hopelessness.
For those who suffer from depression, it can seem impossible to understand what's happening and how to find relief — let alone know where to begin looking for help.
By delving into the depths of what depression is and exploring its various causes, signs, and symptoms, we aim in this blog post to create a better understanding of the disorder so that you can seek help from a depression therapist before it's too late.
What is depression?
According to the National Institute of Mental Health, depression (a major depressive disorder or clinical depression) is a common but serious mood disorder. It causes severe symptoms that affect how someone feels, thinks, and handles daily activities, such as sleeping, eating, or working.
Data by NIMH reflect that an estimated 21 million, or 8.4 percent, of individuals in the United States, had experienced at least one severe depressive episode in 2021, making it one of the most co-occurring disorders in the country. Moreover, suicidal thoughts among adults grew to 4.58 percent (an extra 664,000 persons) in 2022, according to the 'State of Mental Health in America' report from Mental Health America.
Depression is a severe mental health condition affecting adults of any age, gender, or background. It's more than just feeling down in the dumps—intense feelings of hopelessness and guilt characterize depression, withdrawal from social activities and responsibilities, difficulty concentrating, changes in sleep patterns and appetite, physical ailments such as headaches and fatigue, and thoughts about death or suicide.
Unfortunately, for many people suffering from depression, these are all too real experiences. Depression can feel overwhelming to those suffering; however, there is hope! Educating ourselves on what depression entails, the available treatment options, and how we can support those suffering from depression gives us a strong sense of empowerment over our own lives.
Is depression a disability?
Yes and no. The answer depends on your unique experience of depression. It absolutely can, and many people with depression do qualify for disability.
Depression is a complex and challenging condition that affects millions of people worldwide. It impacts individuals in various ways, and it's not uncommon for those experiencing depression to wonder if it qualifies as a disability. While depression can significantly impact a person's daily life and functioning, whether it is considered a disability depends on several factors.
In some cases, depression can meet the criteria for disability as defined by the Americans with Disabilities Act (ADA) or other disability rights legislation in different parts of the world.
The ADA defines a disability as a physical or mental impairment that substantially limits one or more major life activities. This can include activities such as sleeping, concentrating, working, maintaining relationships, and taking care of oneself.
In order to qualify for disability benefits, you’ll have to prove that your depression meets those criteria. This can be done through a primary care practitioner or a therapist.
If you're experiencing depression and it is impacting your ability to work or carry out essential life activities, it is crucial to explore your rights and options. Seeking the support of a qualified mental health professional, such as a therapist or psychiatrist, can provide you with an informed understanding of how depression is affecting your life and whether it meets the criteria for disability accommodations.
Types of Depression

Depression is classified by healthcare practitioners based on its symptoms and causes. These distinct types typically have no discernible reason. They can remain far longer in some persons than in others for no apparent cause. With that said, let us now look at some of the different types of depression:
- Major Depressive Disorder (MDD)
Major depressive disorder (MDD), also called depression, is the most common form of depression. It is a mental condition defined by persistent poor mood, negative self-esteem, and lack of enthusiasm or satisfaction in typically pleasurable activities for at least two weeks, although many people experience it for much longer. Proposed by some US doctors in the mid-1970s, the American Psychiatric Association accepted the name in the 1980 version of the Diagnostic and Statistical Manual of Mental Disorders (DSM-III) for this symptom cluster under mood disorders and has since become extensively used.
- Persistent Depressive Disorder (PDD)
PDD, formerly known as dysthymia, is recognized in patients who experience at least two main depressive symptoms for at least two years. In double depression, it is possible to experience both severe and less severe symptoms and have both PDD and MDD simultaneously. In addition to MDD symptoms, people with PDD can sometimes seem irritable, gloomy, temperamental, or pessimistic. However, it’s important to remember that these are symptoms of a mental health issue and not a personality flaw.
- Bipolar Disorder
Bipolar disorder, formerly known as manic depression, is a psychiatric condition characterized by significant mood fluctuations that elicit emotional highs (mania or hypomania) and lows (depression). Mood swings might occur infrequently or frequently throughout the year. Although bipolar disorder is a chronic illness, many people can control their mood swings and other symptoms by adhering to a treatment plan of both therapy and medication. Bipolar disorder is usually treated with psychological treatment (psychotherapy).
- Seasonal Affective Disorder (SAD)
Seasonal Affective Disorder (SAD) is a type of depression that is triggered by a season. Usually this is winter, when the days get shorter and there’s less light, but a less common form of summer SAD is possible. SAD is connected with variations in the sunshine and is frequently accompanied by excessive sleep, weight gain, and cravings for carbohydrate-rich meals. Fortunately, SAD is highly treatable with a combination of lifestyle changes (like sitting under a sun lamp), therapy, and medication for more severe cases.
- Postpartum (or Perinatal) Depression (PPD)
Postpartum (or perinatal) depression (PPD) is identified in mothers who have significant depressive symptoms immediately after giving birth. A mix of events, including abrupt changes in hormone levels after childbirth, typically causes PPD. Episodes of extreme sadness, worry, or weariness are significantly greater and stay far longer than the transient "baby blues," which are the relatively moderate melancholy and anxiety symptoms many new moms face in the first few days following delivery. Mothers experiencing PPD may also experience postpartum anger. Therapy and medication have been proven instrumental in mothers recovering from PPD quicker.
- Premenstrual Dysphoric Disorder (PMDD)
It is a primary health concern related to premenstrual syndrome (PMS). PMDD produces significant irritation, melancholy, or worry in a week or two before the period. Symptoms often disappear two to three days after menstruation begins.
What Causes Depression?
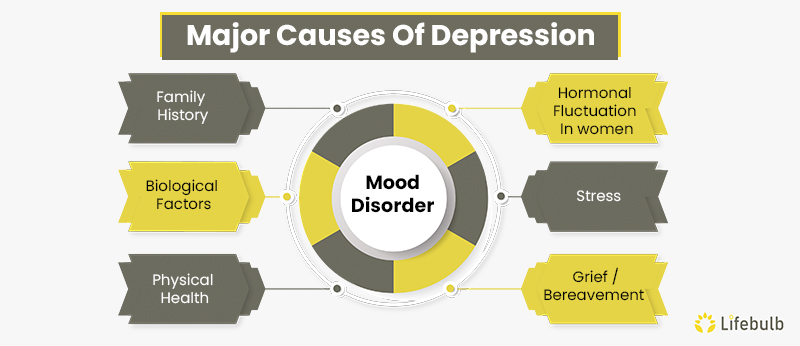
Depression is a complicated and multifaceted condition that affects millions of people worldwide. While the exact causes of depression are still not fully understood, several factors are known to contribute to its development, like a chronic medical condition or a significant life event such as a relocation or the loss of a loved one. Let's understand some of these most common causes of depression.
- Genetics
A history of depression in the family may raise the likelihood of getting a major depressive disorder. Depression is regarded as a complex attribute. Thus, there are several separate genes, each with little influence, rather than one gene contributing to the condition. Depression, like other mental disorders, has more complicated origins than solely genetic diseases like cystic fibrosis.
- Biological Factors
In individuals who struggle with depression, there can be a chemical imbalance in areas of the brain that control mood, thinking, sleep, hunger, and behavior. This is brought on by changes in the affected brain's neurotransmitter levels. Neurotransmitters are chemical compounds that allow various parts of the brain to interact with one another. When particular neurotransmitters are in limited supply, they might result in clinical depression symptoms.
- Physical Health
Chronic illness and depression are linked in more ways than one. The mind and the body are deeply entwined. If someone has a physical health condition, they may also experience changes in their mental health. The stress of having a chronic illness may precipitate a significant depressive episode. For example, thyroid diseases, Addison's disease, and liver conditions can all induce depressive symptoms.
- Hormonal Fluctuations in Women
Researchers say women are twice as likely to suffer from severe depression than men. Since the frequency of depressive episodes rises throughout women's reproductive years, hormonal factors are believed to be at work. Women are more vulnerable to depressive disorders while their hormones are in flux, such as during their menstrual cycle, pregnancy, delivery, and early menopause. After menopause, the risk of depression decreases.
- Stress
Life circumstances that are stressful and overwhelming a person's ability to cope can significantly contribute to depression. Researchers believe that copious amounts of the stress hormone cortisol may disrupt the neurotransmitter serotonin and lead to a depressive episode.
- Grief/Bereavement
Though typical, sadness or grief following the death or loss of a loved one might increase the likelihood of going into depression. Sleeping problems, a loss of appetite, and a loss of pleasure or interest in activities are all natural reactions to loss. Grief symptoms are intended to fade over time. However, when symptoms worsen, grieving may progress to depression.
While the causes of depression are complex and varied, understanding the factors contributing to its development can be an important first step in seeking depression treatment and managing symptoms. Whether through depression therapy or other forms of support, a range of effective treatments are available for depression, and no one has to struggle in silence.
How is Depression Different from Sadness, Grief, or Anger?
Depressive symptoms can show up in other mental health issues and even the everyday blues. So what makes depression different from normal sadness, grief, or anger?
While these emotions are all valid and can be a normal part of the human experience, depression stands apart in its duration, intensity, and impact on daily life.
In order for a depression diagnosis to be given symptoms must be present for at least 2 weeks. This makes it different from the occasional bad day or sadness.
Sadness is a natural response to difficult situations, such as loss, disappointment, or hardship. It often comes and goes in response to specific events and tends to lessen over time as circumstances change.
Grief, on the other hand, is a deep sorrow typically associated with the loss of a loved one. It involves a process of mourning and adjusting to life without the person who has passed away. Depression can absolutely be a part of it, and as we saw above grief can be a trigger for Major Depressive Disorder. However, at its core, grief is something different than depression.
Anger, too, is a common emotion that arises in response to feeling threatened, frustrated, or treated unfairly. While it can be uncomfortable, anger is a natural and necessary part of our emotional repertoire.
Depression, however, goes beyond these transient emotions. It involves persistent feelings of hopelessness, low energy, and a loss of interest or pleasure in activities that were once enjoyable. It may come out of nowhere, even when everything in your life is going well. Individuals experiencing depression may also struggle with changes in appetite, sleep disturbances, and difficulty concentrating. These symptoms can persist for weeks, months, or even longer, significantly impacting a person's ability to function in their day-to-day life.
How Can Depression Be Treated?

When a person is depressed, they may feel powerless. But this does not have to be the case. People can do a lot to fight back, in addition to getting depression therapy and making some lifestyle changes.
Natural depression therapies include changing one's behavior (physical exercise, lifestyle, and even mental patterns). Although natural lifestyle changes can go a long way in helping depression, they often need to be accompanied with medication and/or therapy.
Types of therapy effective in treating depression include:
- Psychotherapy
Psychotherapy, often known as "talk therapy," has been demonstrated to be an effective treatment for patients suffering from depression and other mental illnesses. When people undergo psychotherapy, they speak with a skilled therapist to find and manage the circumstances contributing to their depression. Speaking with a therapist might help an affected person discover coping methods for unpleasant emotions. Family or group therapy sessions may also be beneficial.
- Dialectical Behavior Therapy
DBT is another type of talk therapy that evolved from behavioral therapy. Its primary goal is to assist clients in living a "life worth living" by helping those who have difficulty managing their emotions. Additionally, it encourages them to tackle their problems. Dialectical behavior therapy emphasizes skill development to provide people with the tools they need to deal effectively with their problems. Moreover, DBT assists people in setting and achieving long-term objectives.
- Psychodynamic Therapy
Psychodynamic therapy is a "global treatment" that holistically focuses on the client's perspective. Instead of analyzing the client's deep-seated wants, drives, and aspirations, "problem-based" treatments, such as cognitive behavioral therapy, seek to minimize or eliminate symptoms. The distinction between global and problem-based treatment is not the only feature that distinguishes psychodynamic therapy from other, more widespread types of therapy. Rather than focusing on behavior, psychodynamic therapy interprets mental and emotional processes.
- Group Therapy
Group therapy involves meeting with a therapist and a group of individuals who are also experiencing depression. This kind of therapy provides a supportive environment in which individuals can share their experiences, learn from one another, and receive support and encouragement.
Depression is a treatable condition, and therapy can effectively manage symptoms and improve quality of life. If you or someone you know is struggling with depression, reaching out to a mental health professional can be an important first step in finding the support and treatment needed to recover.
Is Depression Curable?
Yes! Although rates of recovery (and how quickly you recover) largely depend on the severity of the type of depression, most studies agree that around 54% of people will recover from depression within a year without any specific mental health treatment. This means they either treated depression on their own or the depression went away naturally. Specific mental health treatment could mean therapy and medication, among other natural remedies.
Around half of the people with depression recover without any help at all, so the chances are very good that you will recover with the support of talk therapy, medication, and other therapies.
It's important to recognize that depression is not a sign of weakness or a personal failing. It is a real medical condition that can be caused by a range of factors, including genetics, environmental stressors, and brain chemistry. Depression can be a chronic condition that requires ongoing management, but it is also a condition that can be successfully treated.
Wrapping Up
One of the most crucial things someone can do to improve themselves is to stick to their treatment plan. It is easy to become disheartened during the first few weeks of therapy and decide not to continue. All methods of treatment take several months before the results appear.
Sometimes, somebody may feel they're doing considerably better, leading them to discontinue treatment entirely. However, it must be emphasized enough to only discontinue therapy after consulting one's mental healthcare provider. Browse our therapist directory to find a depression therapist near you, or give our team a call and we’ll match you with a depression therapist who will meet your needs.

